PIP Frequently Asked Questions F.A.Q.
Does the Patient need to seek treatment within 14 days of the motor vehicle accident to qualify for PIP Coverage?
To qualify for PIP benefits, injured car accident victims must be treated within 14 days of the accident. If a patient does not qualify for PIP benefits because of the 14-day requirement, medical providers can certainly still provide treatment. Other possible sources of payment are health insurance, cash, and/or a letter of protection from the patient’s personal injury attorney.
What is an Emergency Medical Condition and when can the insurance company properly limit Benefits to $2,500.00?
The Current PIP law allows insurance companies to cap benefits at $2,500 (rather than $10,000) if a medical provider listed in the statute determines that the patient does not suffer from “Emergency Medical Condition” or EMC.
The statue defines an EMC as “a medical condition manifesting itself by acute symptoms of sufficient severity, which may include severe pain, such that the absence of immediate medical attention, could reasonably be expected to result in any of the following:
(1) Serious jeopardy to patient health;
(2) Serious impairment to bodily functions;
(3) Serious dysfunction of any bodily organ or part.
EMC is a hot issue in Florida PIP law, and Florida Litigators has been able to successfully recover medical benefits in excess of $2,500 in cases where insurance companies initially took the position that the patient did not suffer from an EMC and therefore denied reimbursement for medical services. Results may not be typical. You may not have as beneficial a result.
Does an Emergency Medical Condition need to be determined within 14 days?
No. The EMC requirement and the 14-day requirement should not be confused. An EMC determination can be made at any time.
If benefits are denied based on an Independent Medical Examination or a Peer Review, can they be recovered?
Yes! Florida Litigators has successfully recovered benefits that were initially denied based on the results of an independent medical examination (IME) or Peer Review. Results may not be typical. You may not have as beneficial of a result. IME’s are conducted by doctors who regularly work for insurance companies. Insurance companies pay these doctors to conduct IME’s and Peer Reviews. After the insurance company pays the doctor to form an opinion, it may cut off benefits. The credibility of these doctors can be cross-examined in court.
If the Insurance Company says benefits have been exhausted, have they paid $2,500.00 or $10,000.00?
Some insurance companies send correspondence which states that benefits have been exhausted, yet they unscrupulously do not state what amount has been paid. It is important that medical providers look out for this issue and have a PIP attorney review their files.
Can Massage Therapy, Acupuncture, or Manual Therapy be reimbursed?
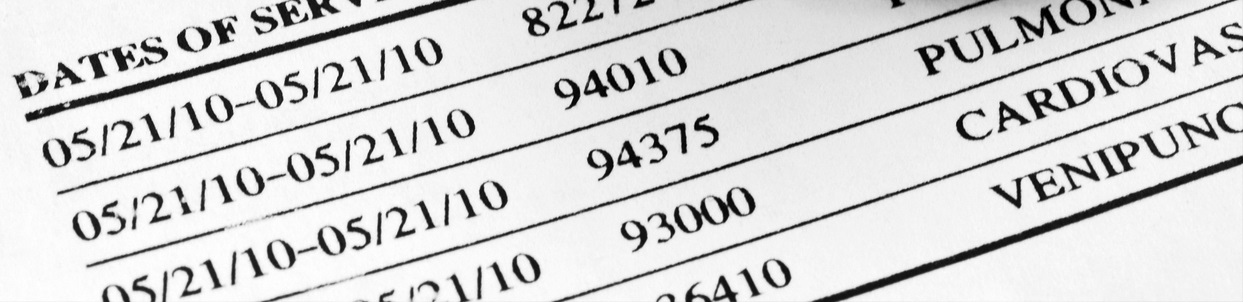
Under the current PIP law, medical benefits do not include massage or acupuncture, regardless of the person, entity, or licensee providing the services. Manual therapy is reimbursable. Some insurance companies are denying claims for manual therapy (CPT Code 97140) and claiming that it is actual massage therapy (CPT Code 97124). This is incorrect. If you have experienced denials for manual therapy, contact a PIP attorney.
Can a Chiropractor determine that a patient sufferes from an Emergency Medical Condition?
No; only a treating medical doctor, an osteopath, a dentist, a physician’s assistant, or an advanced registered nurse practitioner can make an EMC determination.
